PPD– Still a menace
Alina Goldenberg MD, Sharon Jacob MD. Paraphenylenediamine in black henna temporary tattoos: 12-year Food and Drug Administration data on incidence, symptoms, and outcomes. Journal of American Academy of Dermatology. April 201
https://www.jaad.org/article/S0190-9622(14)02217-8/abstract
Review by: Jalal Maghfour and Alina Goldenberg MD
Paraphenylenediamine (PPD) continues to be the main oxidizing agent widely utilized in the US for hair dyeing. One of the major advantages of PPD, particularly in dark shades, is the resulting long-lasting color and the “natural” look that many individuals seek to achieve.
Given that PPD has been recognized as a strong sensitizing agent for several decades, it is solely approved for hair dye use with a concentration limited to 6%.
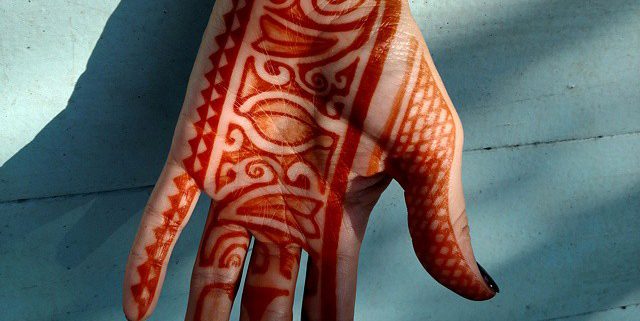
In the past decade, adverse reactions due to PPD have been on the rise; this has been seen primarily when high amounts of PPD is mixed with black henna tattoos, which is a popular form of tattooing among travelers, as it is cheap and easy to remove. The addition of PPD to black henna offers a darker color that is appealing to costumers and enables a faster speeding dyeing process.
Yet, the physical and mental costs associated with local and systemic adverse effects of PPD are high and can be severely debilitating. Herein, the aim of this synopsis is to review the incidence, symptomatology and outcome among PPD-laced henna black tattoo users.
Even though PPD is limited to 6% in hair dye, it has been reported that black henna tattoo products may contain PPD concentrations of up to 30%. It is therefore not surprising that many individuals experience cutaneous reactions to PPD. In majority of cases, allergic contact dermatitis (ACD) including erythema, pruritus, and vesicular/bullous dermatitis may occur (67%). It is important to note that a primary sensitization to PPD is required for ACD to occur following a subsequent re-exposure. In addition, urticarial dermatitis was also reported as an adverse reaction (17%). The latter is a rare form of contact dermatitis that is mediated by an IgE induced mast cell degranulation resulting in hives and wheels. This type of dermatitis is highly concerning as it has been linked to anaphylactic shock.
It is also important to note that beyond localized reactions seen with PPD, systemic toxicity may also occur. Indeed, prolonged cutaneous exposure, at small or large doses for a long period of time, can result in systemic toxicity similar to the toxicity profile reported with PPD ingestion. A wide array of symptoms may be seen and can include the following: angioedema, acute hepatotoxicity, rhabdomyolysis, renal failure, neuropathy, blindness, and death.
Given the spike in severe cases of PPD laced black henna reactions reported by patients worldwide, Dermatitis, the official journal of the American Contact Dermatitis Society (ACDS), has listed PPD as the allergen of the year for 2006. In 2008, both ACDS and American Academy of Dermatology (AAD) officially opposed against the continuous use of PPD-laced black henna. This action has resulted in an increase in both physician and community member awareness as reflected by a lower number of reported cases following the joint ban from highly respected organizations.
This commentary highlights not only the serious adverse effects of PPD but also puts into perspective the central role dermatologists and dermatology organizations can have in public awareness and education by advocating for patients’ safety.