Nickel Contact Dermatitis Summit Webinar
Nickel Contact Dermatitis Summit
For 53 years, nickel has been unparalleled as the most common allergen documented in patch-tested patients of all ages worldwide, which we call attention to as the Nickel Contact Dermatitis Summit approaches. And yet, nickel sensitivity is a much wider problem than the documentation suggests, as Peltonen alarmingly and poignantly pointed out over 30 years ago: “half of the subjects sensitized to nickel have never consulted a doctor because of their nickel dermatitis; still fewer have visited a dermatologist”. In the US we are in the midst of a prospering hidden nickel epidemic akin to that seen in Europe prior to nickel regulation legislation. There are millions of adults and children sensitized each year – the rates are UNACCEPTABLE, because this is a PREVENTABLE cause of allergic contact dermatitis. The Nickel Summit webinar by Dr. Jennifer Chen discusses the impact of nickel allergy in the US and the lack of regulation.
Article Synopsis
Below is a summary of an article speaking more to this topic.
Synopsis by Janna Vassantachart, MD Loma Linda University School of Medicine
Article: Goldenberg A, Vassantachart J, Lin EJ, Lampel HP, Jacob SE. Nickel Allergy in US Adults-A 53-Year Review of Indexed Cases. Dermatitis. 2015 Jul 14.
For 53 years, nickel has been unparalleled as the most common allergen documented in patch-tested US patients of all ages. In 1994, the European Union (EU) decreased rates of sensitization by enacting a Nickel Directive to regulate nickel release to no more than 0.5 µg/cm2/week. No such directive currently exists in the USA.
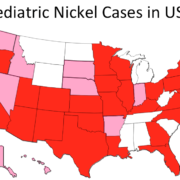
This study conducted a literature review of peer-reviewed adult nickel dermatitis cases published within the United States to identify trends over the past decades, sources of nickel sensitization, and regional variations. It highlights the problem we are encountering at the top of the nickel contact dermatitis summit. The results of the study demonstrated:
- Between 1962 and 2015, there were 74 articles published reporting 18,251 cases of nickel sensitivity in US adults.
- Over the past decades, the frequency of published articles on nickel sensitivity has continuously increased with a significant correlation (r = 0.798, P = 0.057). Compared to only one article published between 1960 and 1970, in the last 5 years, 30 articles have been published.
- Five articles reported occupational exposures such as a stethoscope, chalk, and a military-issued lanyard chain from an identification neck tag (aka ‘‘dog tag’’). The most commonly reported nonoccupational sources were Essure contraceptive microinserts and Amplatzer septal occluders for atrial septal defects.
- Geographically, 27 US states have had at least 1 reported case of adult nickel dermatitis.
Most nickel dermatitis cases seen clinically are neither patch-tested nor captured in the literature, allowing for a prospering hidden nickel epidemic towards the nickel summit. However, this study reveals that even the literature has seen a significant increase in published cases over the past decades. Rising rates of US nickel ACD highlight the need for medical professionals, legislators, and manufacturers to advocate for an EU-like Nickel Directive to regulate the release of free nickel.