Contact Dermatitis Due to Nickel Allergy in Patients Suffering from Non-Celiac Wheat Sensitivity
Original article:
Alberto D’ Alcamo, Pasquale Mansueto, Maurizio Soresi, Rosario Iacobucci, Francesco La Blasca, Girolamo Geraci, Francesca Cavataio, Francesca Fayer, Andrea Arini, Laura Di Stefano, Giuseppe Iacono, Liana Bosco & Antonio Carrocio. Contact Dermatitis Due to Nickel Allergy in Patients Suffering from Non-Celiac Wheat Sensitivity.Nutrients, 2017; Vol. 9(2):103
Reviewed by Sue Min S. Kwon, BS, MSI and Annelise Rasmussen BS, MSII, Loma Linda University.
- As gluten allergy becomes more prevalent and widely-knownin society, patients with cutaneous or gastrointestinal symptoms following wheat ingestion may self-report gluten/wheat allergies, though they do not in fact have celiac disease. Almaco et al. suggested the term “non-celiac wheat sensitivity” (NCWS) to describe patients presenting with these symptoms, rather than non-celiac gluten sensitivity (NCGS), as it is not known which component of wheat causes the symptoms.
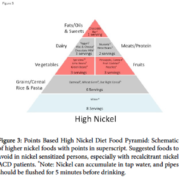
- Non-celiac wheat sensitivity (NCWS) is a relatively new clinical finding associated with gluten-related diseases. Wheat contains nickel, a known contact allergen, which may produce systemic nickel allergy syndrome (SNAS) symptoms. Nickel is the most frequent cause of contact allergy in tested populations.
- NCWS can mimic irritable bowel syndrome (IBS).
- Almacoet al. conducted a double-blind placebo-controlled (DBPC) experiment in order to evaluate the frequency of contact dermatitis due to nickel allergy.
o NCWS patients suffering from nickel allergy were compared with a control group of NCWS patients who did not report nickel allergy.
o NCWS patients with nickel allergy had a significantly higher percentage of atopic disease manifestations than those with irritable bowel syndrome (IBS) and NCWS patients without nickel allergy.
- Nickel allergy (diagnosed by a confirmatory epicutaneouspatch test) may manifest with both cutaneous and gastrointestinal symptoms.
o All NCWS patients with nickel allergy exhibited cutaneous erythema.
o Less than 10% of NCWS patients without nickel allergy exhibited such symptoms.
- Causes may include dietary short-chain carbohydrate load, autoimmune disorders, and non-immunoglobulin E – mediated wheat allergies.
- This study did not allow for evaluation of the frequency of nickel allergy in NCWS; nickel patch testing was only performed on patients who self-reported contact dermatitis. Nickel allergy could have been present in patients who did not report nickel allergy.
- Selection bias was a result of patients referred to tertiary centers.
- Alcamo et al. suggest that patients with NCWS who exhibit cutaneous erythema should be tested for nickel allergy.
http://www.mdpi.com/2072-6643/9/2/103