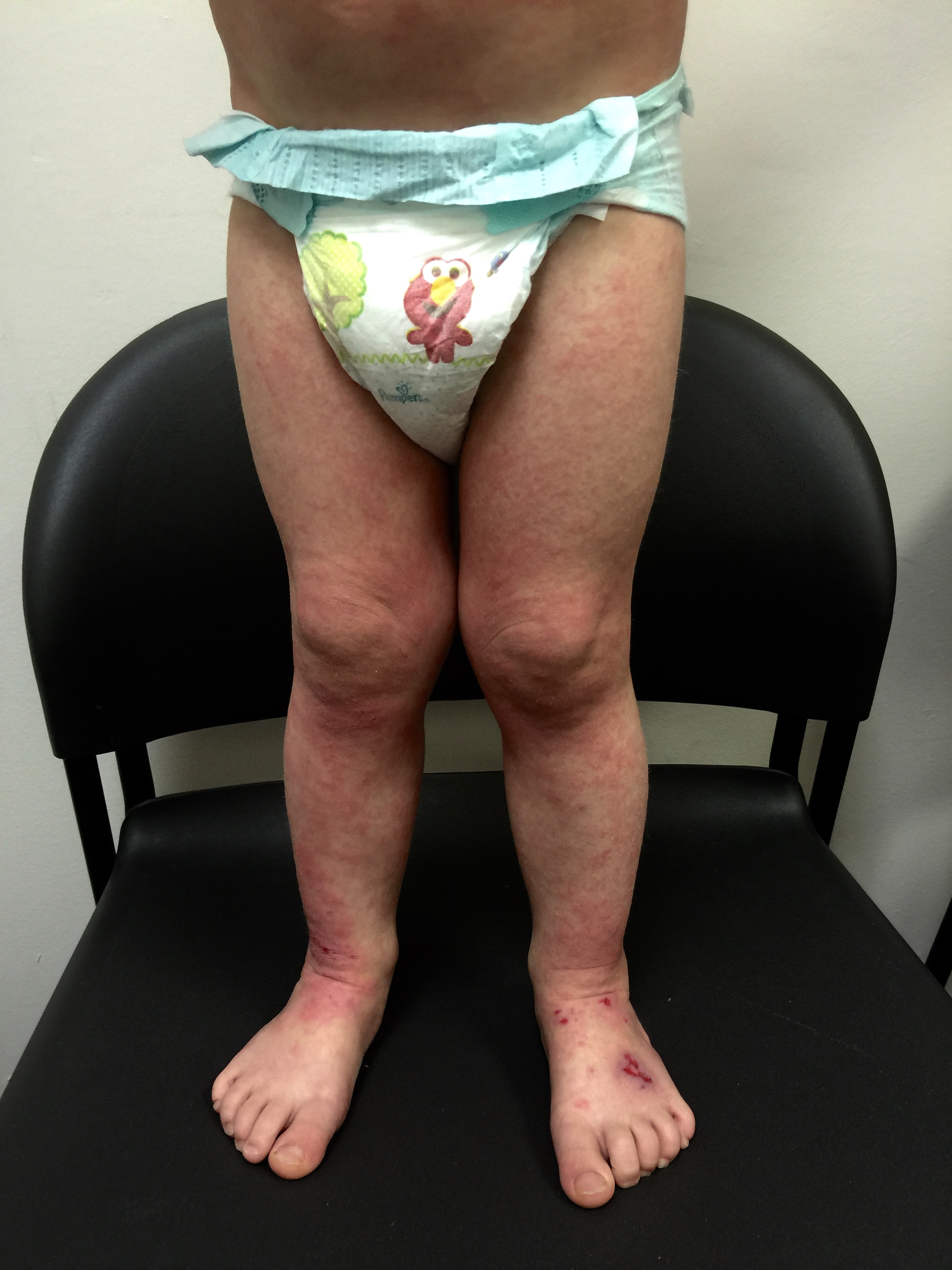
For Helen D., resident of Miami, Florida, the relationship is too close to home. Helen suffers from a disease called allergic contact dermatitis (ACD), which is an allergy to chemicals in the environment. It is a preventable and (through avoidance) treatable disease, yet many people suffer for decades. Others are treated with oral or injected steroids, such as prednisone. While this may make the dermatitis resolve, it is all too great a reality that it returns as the medicine wears off, requiring further treatment. These treatments are not without side effects, and serious ones at that! Steroids can damage the eyes, raise blood pressure, induce diabetes, and even destroy bones. So why not just see the doctor and get cured? It should be that easy, but it can be difficult to diagnose without the appropriate testing tools and expert evaluation.
Helen’s Story
“I have had sensitive skin and allergies “all my life” and have taken allergy medication and shots. I experienced eczema and even had numerous skin cancers removed. To top it off, I am a breast cancer survivor of thirteen years, so I have had my share of medical issues to deal with in my fifty-seven years.
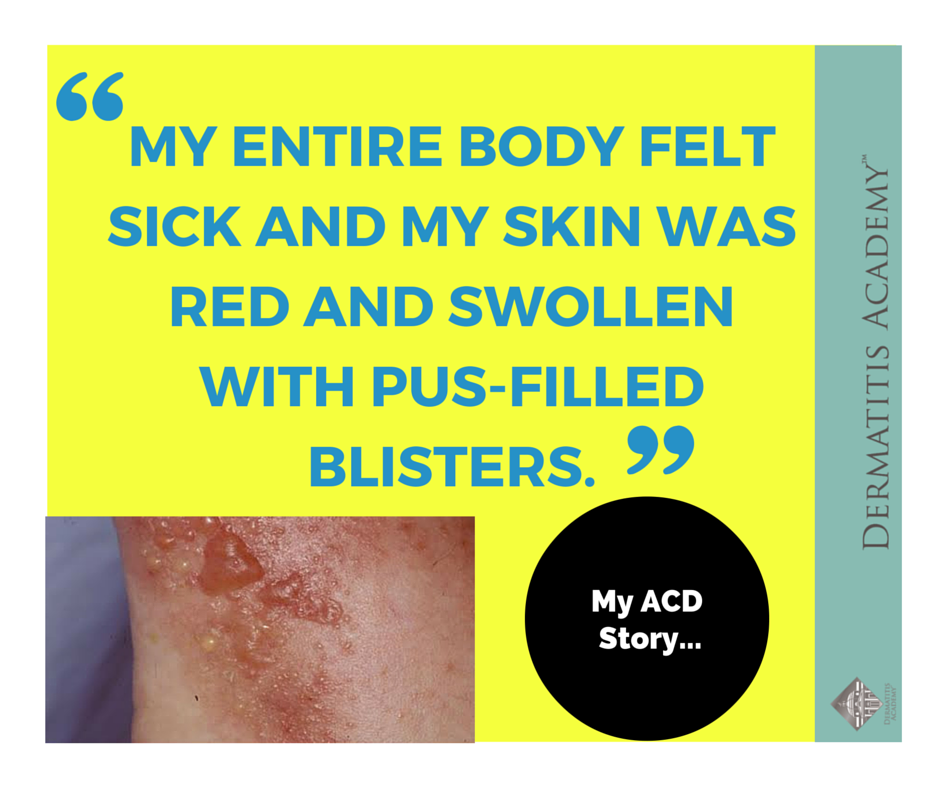
Nothing, however, prepared me for the experience I would be thrust into in February 2003. I was prescribed a well-known statin drug, and after a few days of taking it my face began to itch and rash. On the fifth day I woke up looking like a monster with a bright red, swollen, and indescribably itchy face. I called the General Practitioner who had prescribed the medication and was informed they could not fit me in. I informed them I WAS coming in, and when they saw my face, I was sure they WOULD see me. When the medical assistant slid open the glass door into the patient waiting room, his eyes widened in disbelief with a hint of horror; a look I was to see many times over the next few years from those who witnessed me in a major flareup or saw my “show and tell” photos I took to all appointments for the next two years. The doctor gave me a shot of cortisone and a prescription for a prednisone dose-pack. Over the next few days, the red, swollen and itchy skin was replaced by parched skin that had the consistency of sandpaper and then miraculously turned into clear, fresh dewy looking smooth skin, thanks to steroids.
Thus began a two-year sentence of tortuous skin eruptions and an emotional roller coaster ride. I experienced severe flare-ups, often several times a week. The flare-ups would begin with an itchy face and very rough skin. Then the skin would begin to feel raw and burned, and most ointments or creams felt like pouring alcohol on an open wound. The next phase was peeling, parchment-dry, sandpaper skin that no cream, moisturizer or diaper ointment alleviated. One dermatologist prescribed a soothing mask of fresh cold yogurt followed by Crisco, which provided short-term relief. Several times I was given antibiotics when the inflamed skin became secondarily infected. Despite vast quantities of Benadryl, prescription antihistamines and creams, nothing helped except steroids.
I began my long journey seeking help within the medical community, first seeing my allergist. After seeing my inflamed face, sometimes with bright red circles around my eyes several times, the doctor diagnosed ”allergic contact dermatitis” or ACD,not hives as I had assumed. This was my first introduction to the name of this hideous disease. By March, I had seen my dermatologist and allergist several times and found an endocrinologist, who after many tests, told me I had a compromised immune system, a sluggish adrenal system, and was possibly pre-auto-immune though did not test positive. He put me on a regimen of 10 mg of Medrol (prednisone) for three months and told me it was dangerous to be on longer than this and would also make me gain weight (how true!).

After I was off the prednisone for the appropriate time, my allergist performed a T.R.U.E. Test® (Allergen Patch Test) test, which yielded no results. Perhaps this was because a medical assistant, uneducated in proper patch test reading techniques, administered the test. Also, I was never told to come back on Friday, after the assistant removed the patch on Wednesday. I was still in the dark about what was causing my flare-ups, which continued week after week.
I never knew when I accepted a social invitation, if I would really be able to attend. I missed numerous days at the office, hiding my face or seeing doctors. After many months, I let more and more friends and colleagues see me in a flare up. Often I would burst into tears upon waking up in a full fledged flare up, knowing the impending cycle to come over the next four or five days.
My second allergist also administered a T.R.U.E. Test® (Allergen Patch Test) in August 2003 and discovered I was very reactive to a common preservative, Methylchloroisothiazolinone/ Methylisothiazolinone (MCI/MI). Knowing I was highly allergic to MCI/MI was a big help, as I could begin to examine everything in my medicine cabinet and extensive arsenal of makeup, hair and skin products. I eliminated products and carefully scrutinized all product labels before buying. I read the long list of ingredients on products looking for Methylchloroisothiazolinone or synonyms for MCI/MI.
Sounds fairly simple, but not so fast! I discovered by trial and error and my own amateur investigative work that MCI/MI is in most liquid fabric softeners and some liquid soaps. The ingredients are not listed on these products for competitive purposes. I had begun to notice that every time I went on a business trip and stayed in a hotel, I started to flare up by the second or third day. The dreaded itchy rash returned on my face often accompanied by swollen eyes, a portent of a full flare up to come.I carried “melt in your mouth” children’s Benadryl and would copiously pop them in my mouth at the first sign, to no avail. I carried tinted glasses,so when my eyes began to swell, I could cover them and still help ‘man’ the vendor booth for the company I partially own. When the flare up was bad, I would often call a doctor to get a prescription for a steroid dose pack to alleviate the problem and allow me to finish the trip sans major flare up. Then in August of 2003, we bought a vacation condo. The realtor left a big basket of cleaning products which included liquid fabric softener, something I do not use at home. Lo and behold, after two nights sleeping on the sheets and pillowcase, I began a flare up. This was one of the countless times I racked my brain to figure out what I was using that was “different” or “new” and the liquid fabric softener light bulb lit up!

It was then I discovered that finding product ingredients when they are not listed on the product is not a simple task! The ingredients are not on company web sites and you must put in a request, either in writing or by email and eventually be contacted. You will NOT be provided with a list of ingredients, but will be told IF the substance you ask about is in the product. MCI/MI is in liquid fabric softeners (not sheets) from three major manufacturers I checked with. This is typical of the sleuth work that the patient must go through to eliminate known allergens!
Over eighteen agonizing months, I saw six dermatologists, three allergists and continued to see my endocrinologist searching for answers. I spent thousands of dollars on my portion of numerous medical tests, untold amounts of creams, OTC medications or supplements, acupuncture, products and devices, including an electric hand-held anti-itch device ordered from the Internet. Amazingly, the anti-itch device for $49.99 actually did provide some temporary relief! I switched to organic pest control in my house in an attempt to rid my life of unnecessary chemicals, and began eating organic food whenever possible. I went to a medical intuitive who told me my adrenal system was not working well but gave no good path to recovery. I even tried drinking fresh aloe to cleanse my immune system. At this point, if someone told me rubbing monkey dung on my face would solve the problem, I would have tried this too!
I was on corticosteroids for a 3-month period in 2003, a one-month period in 2004, had at least three cortisone shots and many dose packs. I vaguely knew they had a potential to be dangerous, but desperation and agony usually preceded my requests for this relief. I also knew people with asthma took Prednisone for years.
At some point during my odyssey, I realized via my Internet research that I needed extended patch testing. First I started asking the allergists and the six dermatologists, including one at the Cleveland Clinic, hoping they could either administer the extended patch test, or would know someone (anywhere!) who did. Nada! One allergist had provided the name of a doctor in NYC, whom I was unable to contact. After several months, I printed out a long list of Miami dermatologists from my insurance company web site and began phoning to ask if they performed extended patch testing. Most of the appointment schedulers did not have a clue as to what I was talking about, and I usually had to hold for a nurse, or be called back. Many phone calls later; I eventually hit pay dirt when I called the University of Miami Dermatology Group. The scheduler happened to ask a nurse in the presence of a resident. I was given the name of a contact dermatologist at the University of Pennsylvania. This contact became vital to my eventual diagnosis!
Coincidentally, or by the grace of God, I had a vendor show coming up in Philadelphia three weeks after getting the doctor’s name. It’s amazing what begging can do. The scheduler actually took pity on me when I told her my situation and fit me in May 2004, a full fifteen months after my first bad flare up.
In Philadelphia, The UPenn Contact Dermatologist was very compassionate, saying I must get help as my quality of life was suffering. What an understatement, but at last I had found someone who truly related to my plight! The doctor said he could perform tests in Philadelphia, but I might be more interested in a doctor on the west coast of Florida and I eventually got a blessed appointment for August 4, 2004 in Ft. Myers, Florida.
On a Monday eighteen months after my first bad flare-up, the doctor administered an extended patch test and 206 ingredients were positioned on my back next to identifying numbers and covered with tape. I could not get my back wet for the five-day test duration. On Wednesday, the patches were removed for the first reading and I returned Friday for the second reading. Finally! I was given an extensive list of allergens and directions for following an “avoidance” regimen. Allergens included Bacitracin, Goldsodiumthiosulfate (Gold), Nickel, Fragrance Mixture, Methylchloroisothiazolinone (MCI/MI); Bromonitropropane Diol; Paraphenylenediamine Mix (Black Rubber) PPD; Dermatophagoides mix (Pteronyssinus/Pharinae) – house dust mites. Later, Tetracaine, 2.5 Diaminotoluene Sulfate and Ammonium Persulfate would be added to this list.
Gone was my gold jewelry, replaced by platinum, or silver or stainless steel tested for nickel content. No more hair color, as hair dye contains PPD, one of my major allergens. I changed many personal products including my laundry detergent, my toothpaste and looked for “fragrancefree” products that did not contain my allergens. The flare-ups did not entirely go away, but subsided immensely! On a follow up visit, several months later, I gave my doctor a big hug, telling him he had given me my life back!
My sixth dermatologist informed me in December 2004 that thankfully, Miami now had a dermatologist specializing in allergic contact dermatitis! This was my introduction to Sharon Jacob, MD, Assistant Professor of Clinical Dermatology at the University of Miami, who has been so important in my diagnosis, education and understanding of Allergic Contact Dermatitis. Ironically, that resident in clinic who directed me to the UPenn doctor in the first place had been Dr. Jacob. A marvelous touch of fate provided the help I so desperately needed.
Through Dr. Jacob, I am still learning new ways to avoid allergens each and every day. I learned additional products to avoid. I learned I needed to purge all products from my life that were not “fragrance free.” I had not been strict about “fragrance free”, and consequently when I got serious, I eliminated a large shopping bag full of products from my home. I learned the term “unscented”means yet another chemical has been added to the product to mask the scent. Read product labels and you will see chemicals upon chemicals upon chemicals.
Chemicals have proliferated in our society at an alarming rate. PPD (Paraphenylenediamine) is a good example. Per Dr. Sharon Jacob,“many temporary tattoo artists mix PPD with ‘natural’ henna to give it a brown-black color and to accelerate the fixing time of a temporary henna tattoo. Henna use/tattoos are a growing fad in the under 18-year-old population, as parents generally permit this type of tattooing. Furthermore, occupational and environmental exposures are diverse, as it is also present in black rubber, scuba gear, photographic developers, printing inks, and textile & fur dyes. Important also is the notable cross reactions PPD has with other compounds with para position benzene rings (para-amino benzoic acid (PABA), as in sunscreens, sulfonamides, sulphonylureas, azo dyes for clothing, and ester anesthetics). Because this allergen is on the rise, with new exposures entering the American cultural arena, it has been nominated for 2005 allergen of the year.”
Dr. Jacob also sternly warned me about the dangers of over-use of steroids, as I still had big flare ups when I stayed in hotels and had a prescription for a few more dose packs I would use in desperation.
Sadly Dr. Jacob’s warning came too late! I started having right leg pain around the middle of January 2005. I had just taken a yoga class, so I attributed the pain to a pulled muscle or tendon. The pain worsened, causing me to limp part of the time and have pain every morning. I saw two orthopedics in the beginning of February and one began the process of x-rays,bone scans and MRI’s.By the beginning of March,I was also having pain on my left side, walking with a cane, in lots of pain at night and severe pain in the morning. I still attributed this to a soft tissue injury, and went into major SHOCK when I was given my diagnosis in mid March 2005.
My Diagnosis –bilateral Osteonecrosis or Avascular Necrosis. Loss of blood supply to the bone or increased pressure within the bone causes the blood vessels to narrow; making it hard for the vessels to deliver enough blood to the bone cells and the bone literally necroses or dies.
My Probable Cause –off and on corticosteroid use for a two-year period.
My Treatment – complete hip replacement or hip decompression surgery for both hips!
I am now using crutches or painfully lurching around on a walker and seeking the best orthopedic surgeon to perform my needed surgery and treatment. When the pain is not too bad, I work on the computer from my house, as going into the office is difficult. Friends take me grocery shopping and my over-stressed husband is trying to run a business and take care of chores he never even dreamed of in the past.
In the 19th century, miners carried canaries in small wooden cages down into the mines. The little garden-variety songbirds served as sentinels for miners, warning them by dying or falling off their perch when toxic fumes were in the mineshaft. The cheerful birds were extra sensitive to poisonous gases, so they’d react to them well before the miners, who would then quickly evacuate. People like me with chemical sensitivities have sometimes been referred to as this century’s canaries. What is the proliferation of chemical additives in foods and products doing to our children, our environment and ourselves? Perhaps it is time to heed the warnings of the canaries!
My current orthopedic condition was AVOIDABLE and is a human medical tragedy I will have to make the best of. I am telling my story to prevent someone else from going through what I have, and what I face in the next year. There is a serious lack of education regarding ACD by lay people, doctors, and medical personnel. There is a serious lack of knowledge of the side effects of prednisone. And finally, there is a major lack of access to the patch testing modality. Had the majority of my allergens been diagnosed within the first six months, I would not have taken steroids for two years and would not be facing extensive surgery and orthopedic treatment. This did not need to happen to me and should not happen to anyone else.”
My Allergic Contact Dermatitis (ACD) Story is a portion of the Dermatitis Academy Blog that highlights real life, user submitted, allergic contact dermatitis journeys in an attempt to provide awareness and encouragement regarding this crippling disease.
For more info on allergic contact dermatitis or how to get tested (patch tested), please visit our home page here.
Infographic by Peter Gust