Simple & Free
Simple & Free
By Hannah Hill, MD and Sharon E. Jacob, MD
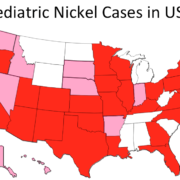
It is time to be Simple & Free! Pediatric allergic contact dermatitis (ACD) has been increasingly recognized in the United States over the last decade. Reported rates of positive patch tests in children referred for suspected ACD range between 27% and 95.6%. Many young children are becoming sensitized to contact allergens found in personal hygiene products such as cleansers, moisturizers, sunscreens and topical medications like steroids and antibiotic ointments. Dr. Jacob and her team have been promoting pre-emptive avoidance strategy (P.E.A.S.) since 2005, especially in patients with widespread dermatitis, and seeing a remarkable impact. This led to the team developing the Simple & Free guideline, making P.E.A.S publicly available, with the goal of reducing skin rashes (dermatitis) associated with the top sensitizing allergens and potentially a decrease in sensitization.
With the goal of identifying the top allergens responsible for a significant portion of pediatric ACD caused by personal hygiene products, Hill et al. reviewed five recent pediatric patch test studies. The top ten allergens identified by this meta-analysis of the US pediatric patch test were neomycin, balsam of Peru (a screening substance for fragrance allergy), fragrance mix, lanolin, cocamidopropylbetaine, formaldehyde, corticosteroids, methylchlorisothiazolinone (MCI)/methylisothiazolinone (MI), propylene glycol, and benzalkonium chloride. Upon review of the included studies it was also estimated that between one quarter and one third of children suffering from ACD could potentially benefit from a “pre-emptive avoidance strategy” (P.E.A.S.) of the stated top 10 allergens! Dermatitis Academy then created the Simple & Free guideline to highlight the products devoid of the top 10 sensitizers. Given that benzalkonium chloride (BAC) is a very rare allergen and well known irritant, the high reporting from one study in the meta-analysis likely represents irritant reactions being read as allergens. For this reason BAC was replaced by para-phenylenediamine, a Consumer Patient Safety Commission (CPSC) designated ‘Strong Sensitizer’, in Dermatitis Academy’s top 10 sensitizers to be pre-emptively avoided.
http://www.ncbi.nlm.nih.gov/pubmed/22828255
http://www.ncbi.nlm.nih.gov/pubmed/18503686
By utilizing resources that identify consumer products for the presence, or lack of, specific contact allergens, consumers can use the pre-emptive avoidance strategy to select Simple & Free formulations and potentially prevent the development of, or remit ACD. Patients most likely to benefit from these efforts include those with eczema, sensitive skin, known allergy, or family history of inflammatory skin diseases. This article briefly shows examples of products devoid of the top allergens, but consumers are encouraged to utilize Dermatitis Academy’s Simple & Free guideline, which utilizes the pre-emptive avoidance strategy P.E.A.S. to highlight products that are both Simple in their formulation and Free of the top 10 P.E.A.S. identified sensitizing allergens.
Article:Hill H, Goldenberg A, Golkar L, Beck K, Williams J, and Jacob SE. Pre-Emptive Avoidance Strategy (P.E.A.S.) – addressing allergic contact dermatitis in pediatric populations. Expert Review of Clinical Immunology. 2016 Jan http://www.ncbi.nlm.nih.gov/pubmed/?term=P.E.A.S.