Parent’s Speak Out About Allergic Contact Dermatitis and Patch Testing

It Just Kept Coming Back
“From a very early age, my daughter had eczema. Hers was a very mild case; sometimes she would get small patches on the back of her knee or on her wrists, other times her skin was perfectly clear. Each night that she had a bath, I made sure to fully moisturize her skin in order to protect it and if needed I would put a small amount of hydrocortisone on affected areas. This usually did the trick and her skin stayed pretty healthy looking. I didn’t want my daughter to suffer from itchy and uncomfortable skin…and I certainly wasn’t going to let that happen. After all it was my job as a mother to keep my child healthy, comfortable and happy. Her skin was great for about 10 years, with a few manageable flares every so often.
As time passed and as my daughter entered upper elementary school, her skin gradually became worse. I continued to treat her skin with the same moisturizer and hydrocortisone cream. Sometimes it would get a little better, but then it would come back worse than the previous flare. She also became much more uncomfortable, it seemed like she was always scratching herself. I noticed more and more scratch marks each day she woke up. We were doing everything that had been suggested…frequent lukewarm baths, pat dry, hydrocortisone, moisturize, a cool temperature in the bedroom, cotton pj’s, and we kept her fingernails short. Still, it got worse.
At one point we had to go to the pediatrician because the backs of her knees were weeping…and it happened seemingly overnight. She was given antibiotic ointment, oral antibiotics, and a new steroid to help calm everything down. Once it calmed down we went back to the same skin care routine.
The condition of her skin continued to decline. The areas around her eyes became dry and scaly at times. It was frustrating trying to apply makeup for dance recitals, as the flakes were so much more visible with her makeup on. Her shins became unmanageable. She literally couldn’t sit still with out scratching or rubbing her legs, back, arms, neck or face. It drove me crazy and I drove her crazy as I told her over and over to stop scratching. She knew she shouldn’t scratch but the itch was unbearable. We had so many battles about her skin…it was seriously affecting our relationship and many nights ended in tears for both of us.
When we first went to see the dermatologist she looked at her skin and asked us questions about what we had been doing to treat the eczema. She said that an injected steroid would help calm things down, so we opted for that. She also prescribed a stronger steroid and a topical immunosuppressant cream for her eyes. She assured us that we were ok to use the steroid cream, and offered advice on tapering down, and which strength of steroid to use on different areas of skin depending on severity of the condition.
Her skin cleared nicely after the shot and the stronger topical steroid. The topical immunosuppressant seemed to work temporarily, but the skin always returned to a flaky and inflamed condition without it. Eventually, the rest of her skin was back to its previous state, and getting worse by the day.
At the next dermatologist appointment, the doctor looked at the condition of the skin and said, “Did you ever have her patch tested?”. I had not heard of patch testing and didn’t know anything about it. She went on to explain that it is a test that can diagnose allergies to substances that she might be coming into contact with that are responsible for creating her dermatitis. She gave me the name of local dermatologist that performs patch testing. We left from the appointment with a few new samples of products, the same treatment plan, and the name of the contact dermatologist.
Did I schedule the patch testing right away? No, I did not. (Looking back I wish I would have dialed that number as soon as we had left that appointment) I thought, “We’ll give it a little more time to see if it clears up.” All the while my daughter was miserable. As I was putting her steroid cream on one night she said, “Mom, are you sure this is making it better?” My quiet and uncertain response was, “It’s supposed to.”
Finally, mid summer, we scheduled a patch test consultation. We met with a nurse practitioner who was under the guidance of the contact dermatologist. She explained the patch test procedure and what my daughter could and couldn’t have as far as topical and oral medications, and also explained the need to limit sun exposure prior to and during patch testing. The dermatologist joined our meeting later and asked us questions about when her condition started, asked if we had trouble with her ears as they had been pierced, and just general questions about possible exposure to allergens. We scheduled my daughter’s patch testing for the week before she would return to school. It would take one full week with four appointments to complete the test, as our insurance required half of the patches to be applied the first day, and half applied at the second appointment, two days later.
I assumed my daughter would want to hang out around the house during patch testing. After all, she was a middle schooler, a vulnerable age for so many girls in regards to appearance. But no, she put on her dance leotard with her patches showing and went to her studio for dance class. She explained to everyone what the patches were and was able to make jokes and laugh about it with her friends.
At our third patch test appointment when both sets of patches had been removed, the doctor indicated that he thought that he would be able to give us some helpful information at the final appointment on Monday. When we got the results at the final appointment, we learned that she was allergic to 10 substances! Nickel, Propylene Glycol, Methylisothiazolinone, Parabens, BHT, Oleamidopropyl Dimethylamine, Lanolin, Octyl Gallate, Bronopol, and Decyl Glucoside. Some of these had elicited stronger reactions than others, but the doctor felt that they were all clinically relevant.
It turns out that many of the substances that she was allergic to were ingredients in the moisturizers, steroid creams, and the topical immunosuppressant cream that we had been using. The very things that we were using to treat her eczema were making it worse! It was explained to us that no one is born allergic to these substances, but through exposure one becomes allergic. So, not only were these ingredients making her skin worse – these substances were in fact responsible for creating the allergic contact dermatitis that my daughter was suffering from. The seemingly hypoallergenic and safe products that I was using on my daughter’s skin, from the time she was a baby, created this nightmare of a condition. When this revelation had time to sink in, I became deeply saddened and outraged.
As I came to grips with all of this new information I began to remove her allergen containing products from our lives and replaced them with “safe for my daughter” products. I learned that in order for my daughter’s skin to have the best chance for healing, we needed to completely avoid all exposure to the substances that she tested allergic to. We changed out personal and household products, eliminating every product that contained her allergens. I changed my products as well so that there wouldn’t be risk of exposure to her from a product that I had used on myself.
As we evaluated every possible place of exposure, my daughter informed me that one of her teachers at school was using an automatic air freshener in the classroom. Air fresheners contain all sorts of contact allergens…and in my daughter’s case, propylene glycol and methyliosthiazolinone would be the worst offenders in this kind of product. She didn’t want me to talk with her teacher about it, as the air freshener was one of the things that he was known for, and he was a popular teacher with the students. I told her that I had to, and it that it was the school’s obligation to provide a safe environment for ALL of the students. I e-mailed her school counselor and she responded with a phone call within an hour of receiving the email. She understood the situation at hand, and immediately suggested to get a 504 plan in place.
At the 504 meeting, I brought my daughter’s binder containing all of the papers we had received at her patch testing appointment. I also showed the teachers and counselors pictures of allergic contact dermatitis reactions. I explained that some of these chemicals are in aerosols and cleaning supplies commonly used at school and at home. The teacher who had the automatic air freshener in the classroom looked up ingredient listings for the household wipes and other cleaning products used at school. It was eye opening for him to see the prevalence of these chemicals in products. As a result of this meeting the educational team had a better understanding of allergic contact dermatitis and they all agreed a 504 plan would be appropriate. We ended up with a comprehensive plan at the end of the meeting. The teachers would use a simple dilute bleach/water solution and paper towels to sanitize and clean desks. The head cafeteria worker would investigate the cafeteria cleaning supplies and report back to us. And the teachers were ecstatic about this one: “Scent Free Zone” signs would hang on the walls of the halls and classrooms in my daughter’s wing of the building. The teachers were excited about the possibility of the elimination of body spray being applied by the boys in the locker hallways. The teachers were very accommodating and I couldn’t have been more pleased with their response.
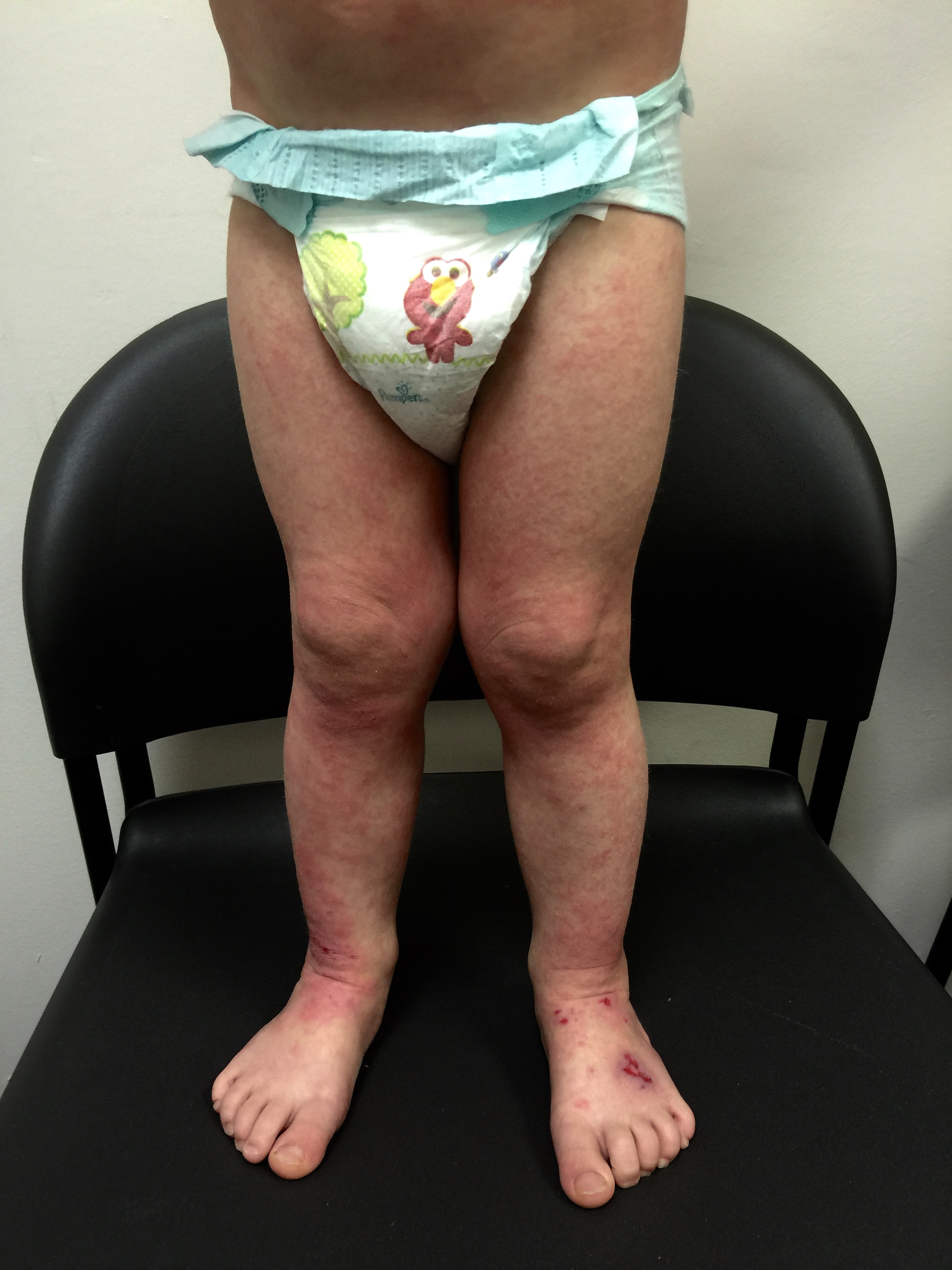
Before/After…


Through continued avoidance of my daughter’s contact allergens, and with time allowed for healing, her skin looks better than it has in many years, and more importantly, she is more comfortable than she has been in many years. I realize now the significance of that one simple question that our dermatologist asked: “Did you ever have her patch tested?” If she hadn’t mentioned patch testing, my daughter would likely still be suffering today. Patch testing, diagnosis, and removal of allergens has been the key to my daughter’s recovery.”
- By Misha B.
- Infographic by Peter Gust
Parents Speak Out About Allergic Contact Dermatitis (ACD) is a special category in the Dermatitis Academy Blog where passionate parents reveal a personal look their family’s journey in dealing with ACD and the role of the patch testing.
Please visit our home page HERE for more information on allergic contact dermatitis. Please share this post in order to create awareness for this seldom considered, but highly relevant disease process.